What is a vaginal pessary?
A vaginal pessary is a device which can be inserted in the vagina to control prolapse. It is made of latex, silicone or vinyl.
Why do I need a vaginal pessary?
Vaginal pessaries usually control the problems associated with prolapse of the vagina and/or uterus. This option avoids surgery
and is especially suitable for patients who wish to have more children, or those who have social circumstances or medical conditions that
prevent them from having surgery. Pelvic organ prolapse can cause sense of bulge, discomfort, urinary and bowel problems as well as sexual difficulties. The device is used as a temporary measure before surgery or as an alternative to surgery.
How does a vaginal pessary work?
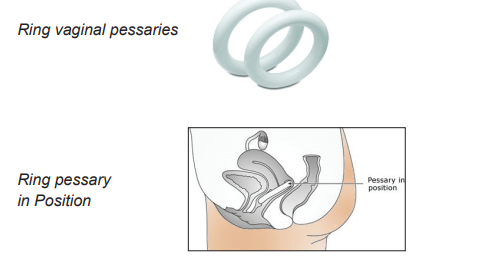
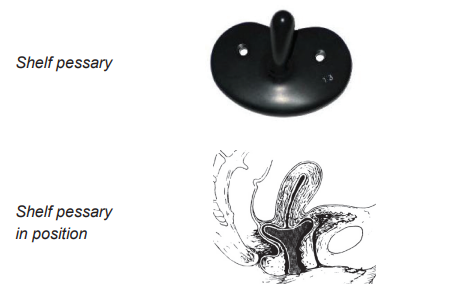
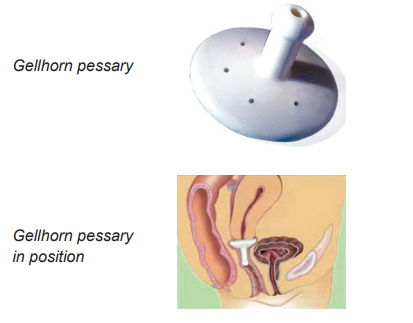
A vaginal pessary is placed inside the vagina. It will stretch its walls and hold the soft tissues up, so as to prevent the uterus or the vaginal walls from bulging out of the vagina. Occasionally for patients with very weak pelvic floor muscles, the pessaries may not stay in place. Your doctor will discuss this with you.
What types of vaginal pessary are available?
Ring pessaries are rounded and soft. They do not prevent you from having sexual intercourse.
Shelf pessaries are like a saucer with a knob underneath. They are hard and do stop you from having sexual intercourse.
Gellhorn pessaries are similar to the shelf style but are soft. They prevent you from having sexual intercourse.
All come in different sizes and the right size is judged on examination. This is like trying a pair of shoes and a number might be tried before
the right size is identified.
Which type of pessary will suit me?
Usually, ring pessaries are tried first. If your pelvic floor muscles are not strong enough to hold the ring in place, you will be able to try other styles. You can discuss the best option for you with your doctor.
What happens after I have had the pessary fitted?
You will be asked to test the pessary by taking a short walk to make sure that the pessary does not cause you any discomfort or slip.
You will be advised to go to the toilet, to make sure it doesn’t prevent you from passing urine. If the pessary falls out or feels tight
or uncomfortable, it will be replaced with a larger or smaller one accordingly.
What about follow up?
The pessary needs to be replaced and the doctor will check it is working properly for you every six months. If you have any concerns at any point, you can call the surgery and book a GP appointment.
What are the risks?
There are risks but these are rare.
Ulceration:
The pessary can sometimes push into the vagina and cause an ulcer or a raw area. The ulcer can get bigger and the pessary may cut
through the bladder or rectum, with potential serious complications. For this reason, pessaries are checked and re-inserted regularly.
The check is carried out using a speculum (like having a smear) after removing the pessary. If an ulcer is detected, the pessary is not replaced. Patients are given oestrogen cream to apply to the ulcer to encourage healing. You will then be asked to return for a check-up 2-4 weeks later. If healing is complete, the doctor will be able to insert a new pessary.
Bleeding:
You may experience some bleeding as a result of an ulcer in the vagina. The vagina will be checked using a speculum, similar to having a smear test. It might be necessary to rule out anything wrong in the uterus, usually by an ultrasound scan.
Moved or slipped pessary:
Occasionally the pessary is too small or the prolapse may be getting worse. Sometimes the pelvic floor muscles are not strong enough; in which case surgery may be a better option for you.
Difficult removal:
Sometimes it can be difficult to remove and replace the pessary. You may need anaesthetic to reduce the pain associated with this, you can discuss this with your doctor.